- January 13, 2025
- Posted by: admin
- Category: Uncategorized

Introduction
DME providers often treat credentialing vs contracting as interchangeable terms, but they are two distinct processes, each critical to a provider’s success. Confusion between the two can lead to mismanaged workflows, delayed reimbursements, and even lost payer opportunities.
Credentialing ensures you’re recognized as a qualified provider, while contracting secures your ability to be reimbursed for services rendered. Together, they form the backbone of your payer relationships and revenue streams.
In this blog, we’ll break down the key differences between credentialing and contracting, explain their roles in driving long-term growth, and provide actionable steps to optimize both processes.
What Is Credentialing?
Credentialing is the process of verifying that a provider meets the necessary qualifications to deliver healthcare services. This includes:
- Education and Training Verification: Confirming degrees, certifications, and licenses.
- Work History and Background Checks: Ensuring providers have the appropriate experience and a clean record.
- Payer-Specific Requirements: Meeting unique standards set by individual insurance companies or government programs.
When Credentialing Is Required:
- Adding a new provider to your team.
- Expanding your network with new payers.
- Renewing or re-credentialing to maintain compliance.
What Is Contracting?
Contracting involves negotiating and signing agreements with payers to define reimbursement rates and terms. Key components of contracting include:
- Fee Schedules: Specifying the rates at which services will be reimbursed.
- Authorization Requirements: Outlining prior-authorization needs for certain DME items.
- Claim Submission Guidelines: Detailing how claims should be submitted for payment.
When Contracting Is Required:
- Establishing a relationship with a new payer.
- Renegotiating existing contracts to improve terms.
- Adding new services or product lines that require payer approval.
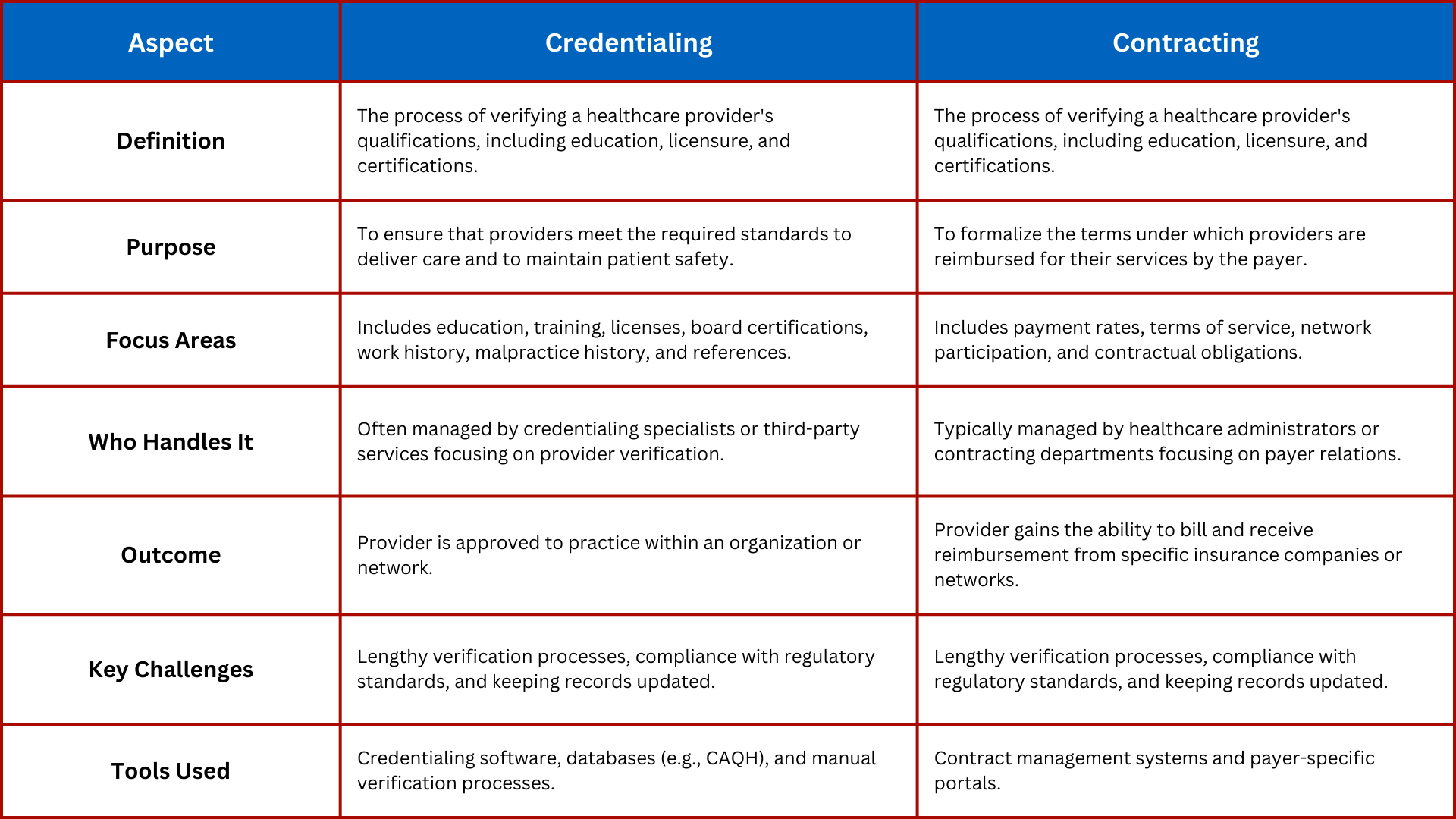
The Key Differences Between Credentialing and Contracting
Why Both Are Essential for Long-Term Growth
- Credentialing Without Contracting Equals No Reimbursement
Even if you’re credentialed, without a contract, you cannot bill or receive payment from payers. - Contracting Without Credentialing Delays Payment
Payers won’t process claims if a provider isn’t credentialed, causing revenue disruptions. - Together, They Drive Network Expansion
Credentialing ensures you meet payer standards, while contracting locks in the financial terms necessary for sustainability. - Both Impact Revenue Cycle Management (RCM)
Credentialing delays or contracting errors can slow reimbursement cycles, directly impacting cash flow.
Actionable Steps to Optimize Credentialing and Contracting
Streamline Credentialing First
- Use a credentialing management system to track provider data and automate reminders for renewals.
- Proactively gather all necessary documents to prevent delays.
Build a Contracting Playbook
- Maintain a database of payer-specific requirements, including fee schedules and submission guidelines.
- Review contracts annually to ensure terms remain competitive.
Coordinate Between Teams
- Ensure your credentialing and contracting teams work together seamlessly.
- Establish a shared timeline for both processes to avoid overlaps or delays.
Outsource When Necessary
- If your team is overwhelmed, consider outsourcing to experts who specialize in both credentialing and contracting.
- Leverage professional services like WWS for multi-payer network expansion.
How WWS Can Help
WWS provides end-to-end solutions to ensure your credentialing and contracting processes are seamless and efficient.
- Credentialing Expertise: From verifying provider data to ensuring payer-specific compliance, we handle it all.
- Contracting Support: Our team negotiates favorable terms with payers, ensuring you maximize reimbursements.
- Integrated Solutions: We align credentialing and contracting workflows to minimize delays and maximize revenue.
Ready to optimize your credentialing and contracting? Schedule a consultation with WWS today:
Schedule a Meeting with WWS.
Conclusion
Credentialing and contracting are two sides of the same coin—essential processes that together form the foundation of your DME business. By understanding their unique roles and integrating them effectively, you can expand your network, secure better reimbursements, and drive long-term growth.
Let WWS take the complexity out of credentialing and contracting. Schedule your consultation today!