Introduction
A successful credentialing process requires more than just meeting payer requirements—it demands a well-structured and efficient team. With the right people in the right roles, supported by robust workflows, your credentialing team can eliminate delays, minimize errors, and enhance revenue cycle management.
In this blog, we’ll outline the key roles and responsibilities of a credentialing team, best practices for building and training your staff, and strategies for maintaining efficiency as your organization grows.
Key Roles in a Credentialing Team
- Credentialing Coordinator
- Responsibilities:
- Manage provider applications and ensure compliance with payer requirements.
- Track licensure renewals, certifications, and re-credentialing deadlines.
- Communicate with payers to resolve application issues.
- Best Fit: Detail-oriented individuals with strong organizational and communication skills.
- Responsibilities:
- Credentialing Specialist
- Responsibilities:
- Conduct initial verifications of provider qualifications, including education, work history, and licenses.
- Audit documentation to ensure accuracy and completeness.
- Handle payer-specific requirements and maintain provider data.
- Best Fit: Experienced professionals familiar with payer standards and regulatory compliance.
- Responsibilities:
- Compliance Officer
- Responsibilities:
- Oversee adherence to federal, state, and payer regulations.
- Update credentialing policies to align with evolving standards.
- Conduct internal audits to ensure ongoing compliance.
- Best Fit: Professionals with a background in healthcare compliance and risk management.
- Responsibilities:
- Technology Manager
- Responsibilities:
- Implement and maintain credentialing management software.
- Automate workflows to track deadlines and ensure timely submissions.
- Generate reports to monitor team performance and identify bottlenecks.
- Best Fit: Tech-savvy individuals with expertise in healthcare systems and data management.
- Responsibilities:
- Payer Relations Specialist
- Responsibilities:
- Build and maintain relationships with payer representatives.
- Negotiate contracts and address credentialing-related disputes.
- Serve as the liaison between your organization and payers.
- Best Fit: Strong communicators with negotiation skills and knowledge of payer policies.
- Responsibilities:
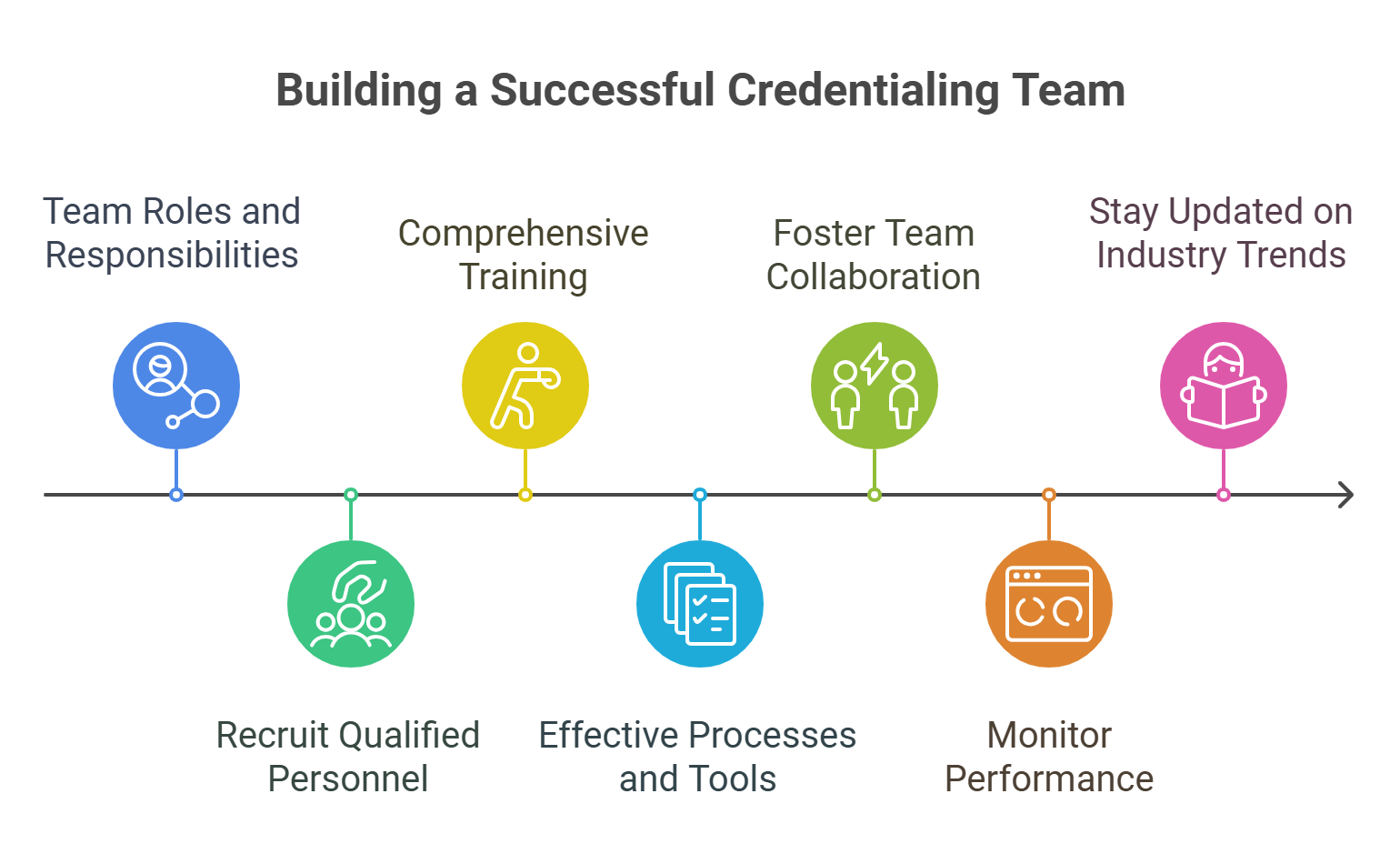
Best Practices for Building and Managing Your Credentialing Team
- Define Clear Roles and Responsibilities
- Why It Matters:
Avoids overlap and confusion while ensuring accountability for each step in the credentialing process. - How to Do It:
- Create detailed job descriptions for each role.
- Assign specific tasks to team members based on their expertise.
- Why It Matters:
- Invest in Training and Development
- Why It Matters:
Keeps your team updated on regulatory changes and payer requirements. - How to Do It:
Schedule regular training sessions on industry standards, software tools, and compliance updates.
- Why It Matters:
- Leverage Technology for Efficiency
- Why It Matters:
Reduces manual work and minimizes errors. - How to Do It:
Implement credentialing software to automate tasks like document tracking, reminders, and reporting.
- Why It Matters:
- Foster Collaboration Across Departments
- Why It Matters:
Enhances communication and ensures alignment between credentialing, billing, and operations teams. - How to Do It:
Use shared platforms or dashboards to keep everyone informed about credentialing progress and deadlines.
- Why It Matters:
- Conduct Regular Performance Reviews
- Why It Matters:
Identifies areas for improvement and celebrates team successes. - How to Do It:
Set measurable goals, such as reduced denial rates or faster credentialing timelines, and review progress quarterly.
- Why It Matters:
Scaling Your Credentialing Team as Your Organization Grows
- Delegate by Region or Payer
Assign team members to specific regions or payers to streamline workflows and improve efficiency. - Use Metrics to Monitor Workload
Track KPIs like approval timelines and application volumes to determine when additional hires or resources are needed. - Partner with Credentialing Experts
Outsource complex or high-volume tasks to experts like WWS to reduce internal workload and maintain quality.
How WWS Can Help
Building and managing an efficient credentialing team doesn’t have to be overwhelming. At WWS, we provide:
- Team Training: Comprehensive onboarding and education to ensure your team meets payer and regulatory standards.
- Technology Solutions: Tools to automate credentialing workflows and track team performance.
- Supplemental Support: Additional resources to handle peak workloads or complex cases.
Schedule a consultation with WWS today to optimize your credentialing team:
Schedule a Meeting with WWS.
Conclusion
A well-organized credentialing team is the backbone of a successful DME practice. By defining roles, leveraging technology, and investing in training, you can ensure your team operates efficiently and stays ahead of payer and compliance requirements.
Ready to build or optimize your credentialing team? Partner with WWS and schedule your consultation today!