Introduction
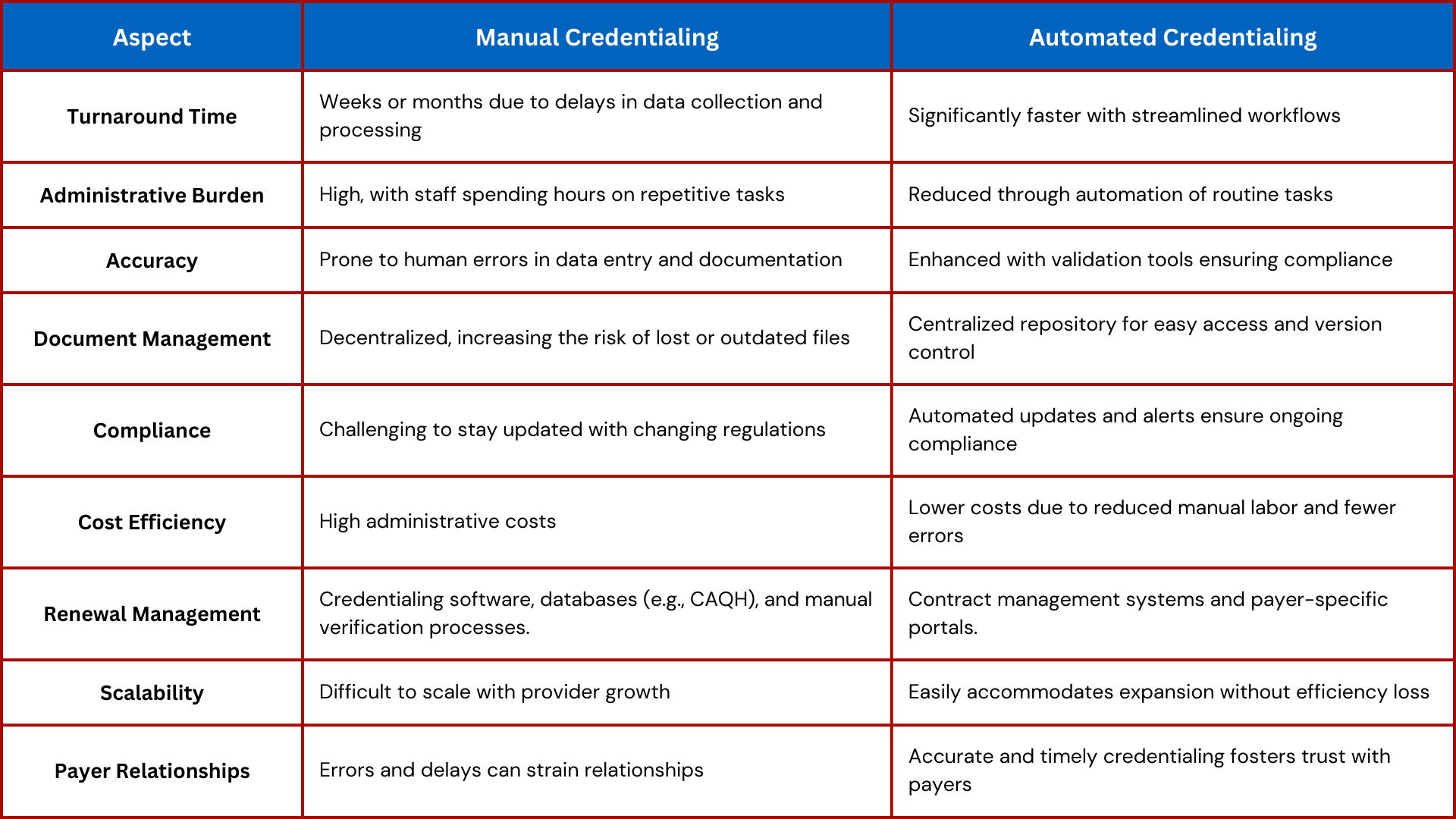
Manual credentialing processes are no longer sufficient in today’s fast-paced DME environment. The constant juggling of payer requirements, deadlines, and provider data creates inefficiencies, increases errors, and slows revenue cycles.
Enter credentialing automation—a game-changer for providers looking to save time, reduce errors, and maintain compliance. In this blog, we’ll explore the benefits of credentialing automation, key tools available in the market, and best practices for implementing automation in your workflow.
Why Automation Is Critical for Credentialing
- Saves Time
- Manual data entry and follow-ups consume significant administrative hours.
- Automation handles repetitive tasks, freeing up staff for higher-value activities.
- Reduces Errors
- Human error is a leading cause of credentialing delays and denials.
- Automated systems ensure accuracy by flagging inconsistencies and missing data.
- Improves Compliance
- Credentialing automation tools track payer-specific requirements and send timely reminders for renewals.
- Accelerates Revenue Cycles
- Faster approvals mean quicker billing and reimbursements.
Top Tools for Credentialing Automation
Modio Health
- Features:
- Centralized provider data management.
- Automated reminders for re-credentialing deadlines.
- Real-time updates on application status.
- Best For: Practices needing a user-friendly interface for multi-provider credentialing.
CAQH ProView
- Features:
- Standardized credentialing application accepted by many payers.
- Secure data sharing across networks.
- Best For: Practices looking to streamline initial credentialing processes.
CredentialStream by Verity
- Features:
- AI-powered credentialing and payer enrollment.
- Real-time analytics to identify bottlenecks.
- Best For: Large DME providers requiring advanced reporting capabilities.
Kareo Credentialing
- Features:
- Automated credentialing for smaller practices.
- Integration with billing systems for seamless operations.
- Best For: Small to mid-sized providers looking for an all-in-one solution.
IntelliSoft Group’s IntelliCred
- Features:
- Comprehensive credentialing and privileging software.
- Flexible configuration for custom workflows.
- Best For: Providers with complex credentialing requirements.
Best Practices for Implementing Credentialing Automation
- Assess Your Needs
- Identify your bottlenecks: Is it data entry, renewal tracking, or payer follow-ups?
- Choose tools that address your specific pain points.
- Invest in Training
- Ensure your team is trained to use the new platform effectively.
- Provide ongoing support as they adapt to automated workflows.
- Integrate with Existing Systems
- Connect your credentialing tool with billing and practice management systems for seamless operations.
- Customize for Payer Requirements
- Set up workflows tailored to payer-specific guidelines and timelines.
- Monitor and Optimize
- Regularly review system performance and make adjustments as needed.
- Use analytics to identify new opportunities for efficiency.
How WWS Can Help
At WWS, we simplify credentialing with a combination of cutting-edge tools and expert support:
- Technology Integration: We help you choose and implement the right automation tools for your practice.
- Customized Workflows: Our team tailors automation processes to meet payer-specific requirements.
- Comprehensive Support: From training to troubleshooting, we ensure your team gets the most out of your investment.
Schedule a consultation with WWS today to transform your credentialing process with automation:
Schedule a Meeting with WWS.
Conclusion
Credentialing automation isn’t just a convenience—it’s a necessity for DME providers aiming to stay competitive. By adopting the right tools and practices, you can save time, reduce errors, and ensure compliance across all payer networks.
Ready to take your credentialing process to the next level? Partner with WWS and schedule your consultation today!