Introduction
For DME providers, credentialing with commercial payers can feel like navigating a maze. Each payer has its own requirements, forms, and timelines—leaving even seasoned teams struggling to keep up.
From delays in application approvals to requests for additional documentation, payer-specific challenges can directly impact your revenue cycle and network expansion goals.
In this blog, we’ll dive into the unique credentialing requirements of top commercial payers, uncover common roadblocks, and provide actionable solutions to streamline the process.
Why Payer-Specific Credentialing Is Challenging
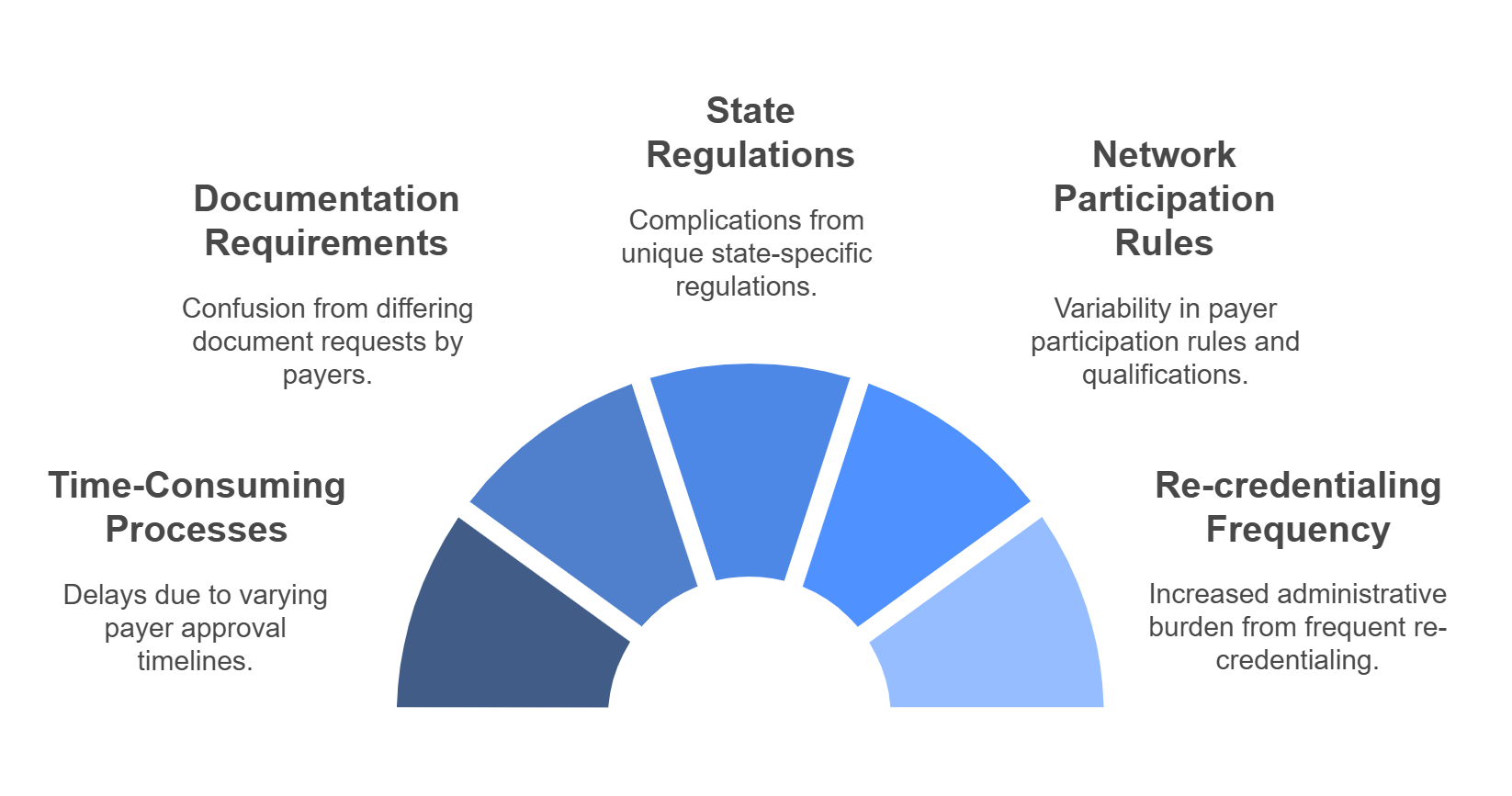
Credentialing requirements vary widely among payers. Some of the biggest challenges include:
- Inconsistent Processes: Each payer uses its own system, creating administrative burden.
- Additional Documentation Requests: Payers may require specific licensure, certifications, or supplemental forms that aren’t standardized.
- Long Approval Timelines: Some payers take months to approve credentialing applications, delaying reimbursements.
- Re-Credentialing Complexity: Keeping track of varying renewal timelines across multiple payers can lead to lapses in approval.
Top Commercial Payers and Their Credentialing Nuances
- UnitedHealthcare (UHC)
- Common Challenges:
- Requires detailed information on provider locations, making multi-site operations more complex.
- Missing even a single document results in application rejection.
- Tips to Overcome:
- Use UHC’s Provider Portal to monitor credentialing status.
- Submit comprehensive applications with all required documentation upfront.
- Common Challenges:
- Blue Cross Blue Shield (BCBS)
- Common Challenges:
- Credentialing timelines vary by state, as BCBS operates through state-level affiliates.
- Fee schedules and contract terms often differ between regions.
- Tips to Overcome:
- Work directly with the local BCBS affiliate for region-specific requirements.
- Maintain an updated checklist of state-specific criteria.
- Common Challenges:
- Aetna
- Common Challenges:
- Strict re-credentialing deadlines can lead to deactivation if missed.
- Aetna often requests supplemental forms beyond the CAQH application.
- Tips to Overcome:
- Set automated reminders for re-credentialing deadlines.
- Prepare and submit all supplemental forms promptly.
- Common Challenges:
- Cigna
- Common Challenges:
- Slow application processing times, often exceeding 90 days.
- Demands frequent updates to provider rosters for multi-site practices.
- Tips to Overcome:
- Follow up with Cigna regularly to check application status.
- Assign a dedicated team member to manage provider roster updates.
- Common Challenges:
Actionable Solutions to Streamline Credentialing
- Create a Payer-Specific Credentialing Matrix
- What It Includes:
- Required documentation for each payer.
- Timeline expectations and contact details for follow-ups.
- Pro Tip: Update the matrix quarterly to reflect changes in payer requirements.
- What It Includes:
- Automate Renewal Tracking
- Use credentialing software to set reminders for payer-specific re-credentialing deadlines.
- Automate notifications to avoid lapses in network participation.
- Follow Up Proactively
- Don’t wait for payers to contact you about missing documents.
- Establish a routine follow-up schedule to ensure applications are progressing.
How WWS Can Help
Navigating payer-specific credentialing challenges doesn’t have to be overwhelming. WWS specializes in simplifying the process with tailored solutions:
- Customized Payer Strategies: We analyze each payer’s requirements to ensure your applications are accurate and complete.
- Automation Tools: Our credentialing systems track deadlines, automate follow-ups, and keep your team on track.
- Expert Support: From application submission to re-credentialing, our team handles the heavy lifting so you can focus on patient care.
Schedule a consultation with WWS today to overcome credentialing hurdles with ease:
Schedule a Meeting with WWS.
Conclusion
Credentialing with commercial payers can be daunting, but with the right tools and strategies, you can streamline the process and minimize delays. By understanding payer-specific nuances, proactively tracking deadlines, and leveraging expert support, you’ll ensure your DME practice thrives in any network.
Ready to simplify credentialing with top payers? Partner with WWS today and schedule your consultation!