Introduction
DME providers operate in a dynamic healthcare environment where unexpected changes—such as provider departures, rapid expansions, or payer network shifts—can disrupt operations and credentialing workflows. Managing these transitions effectively is critical to avoiding revenue interruptions, maintaining compliance, and minimizing patient impact.
In this blog, we’ll explore how to handle provider transitions and other urgent changes in credentialing with efficiency and precision.
Common Scenarios That Disrupt Credentialing
- Provider Turnover
- Challenge: Sudden departures leave gaps in payer networks, delaying billing and reimbursements.
- Solution: Develop a transition plan to quickly credential replacements and maintain payer relationships.
- Rapid Expansion or New Service Lines
- Challenge: Scaling operations or adding new services creates additional credentialing demands.
- Solution: Prioritize payer requirements for new providers or services to streamline onboarding.
- Payer Network Changes
- Challenge: Payers adjust network requirements, forcing providers to update credentialing records or face delisting.
- Solution: Monitor payer communications and proactively address network updates.
- Emergency Situations
- Challenge: Crises like natural disasters or pandemics may require temporary credentialing for new providers.
- Solution: Leverage emergency credentialing programs or waivers to ensure continuity of care.
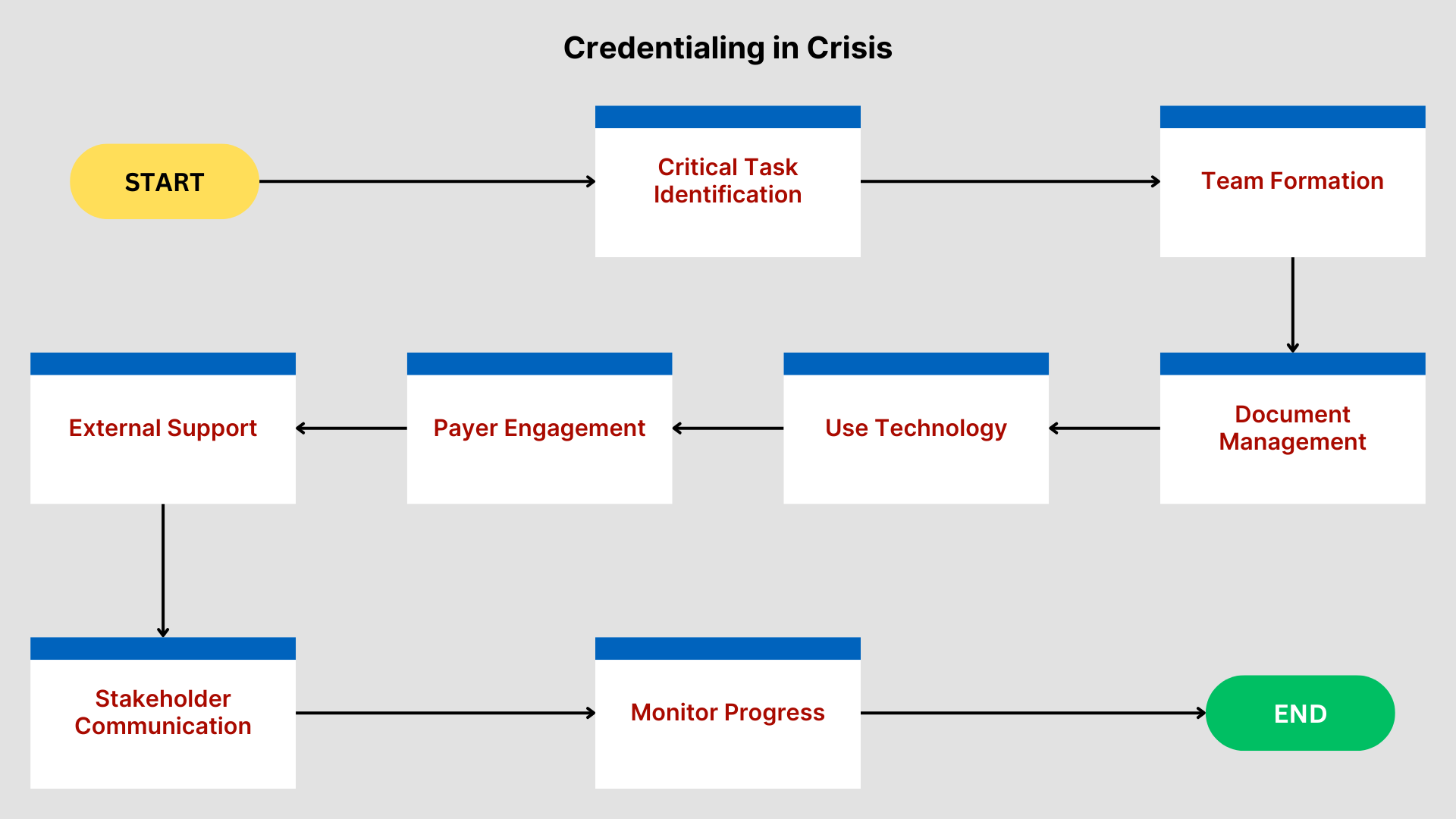
Strategies for Managing Urgent Credentialing Needs
- Develop a Crisis Credentialing Playbook
- Why It Works:
Having a pre-established plan ensures a swift response to unexpected changes. - How to Do It:
- Outline procedures for common scenarios like provider turnover, emergency credentialing, and payer updates.
- Assign team members specific roles to expedite transitions.
- Why It Works:
- Centralize Credentialing Documentation
- Why It Works:
Easily accessible records accelerate re-credentialing and new applications. - How to Do It:
Use credentialing management software to store and organize provider files, payer contracts, and compliance records.
- Why It Works:
- Leverage Temporary Privileges and Expedited Processes
- Why It Works:
Many payers and accrediting bodies offer expedited credentialing or temporary privileges during emergencies. - How to Do It:
Familiarize your team with payer-specific expedited processes and keep documentation ready for submission.
- Why It Works:
- Communicate Proactively with Payers
- Why It Works:
Keeping payers informed reduces delays and prevents misunderstandings. - How to Do It:
- Notify payers immediately of provider transitions or urgent credentialing needs.
- Request extensions or waivers if necessary to maintain compliance.
- Why It Works:
- Automate Tracking of Credentialing Timelines
- Why It Works:
Automation reduces errors and ensures you meet deadlines even during high-pressure situations. - How to Do It:
Use tools that send alerts for upcoming expirations, application deadlines, and payer requirements.
- Why It Works:
Case Study: Managing Emergency Credentialing During a Provider Shortage
The Challenge:
A DME provider experienced an unexpected provider shortage during a regional disaster, resulting in delayed services and potential revenue loss.
The Solution:
- Activated their crisis credentialing playbook, which included a workflow for temporary privileges.
- Submitted emergency credentialing applications with complete documentation to multiple payers.
- Leveraged automation to track application statuses and notify staff of approvals.
The Result:
- Secured temporary privileges for replacement providers within 48 hours.
- Minimized disruption to patient care and avoided significant revenue loss.
Key Takeaway:
A proactive, well-documented plan ensures you can respond quickly and effectively to unexpected challenges.
How WWS Can Help
At WWS, we specialize in managing credentialing during transitions and urgent situations:
- Crisis Credentialing Support: We help you navigate temporary privileges, emergency credentialing, and expedited processes.
- Documentation Management: Our centralized systems ensure your records are always organized and accessible.
- Proactive Planning: We develop tailored playbooks to prepare your practice for unexpected changes.
Schedule a consultation with WWS today to streamline your crisis credentialing strategy:
Schedule a Meeting with WWS.
Conclusion
Provider transitions and urgent changes don’t have to derail your operations. With a proactive approach, centralized documentation, and clear communication, you can manage credentialing challenges effectively and maintain continuity of care.
Partner with WWS to navigate urgent credentialing needs with confidence—schedule your consultation today!