Introduction
Credentialing delays can be a frustrating roadblock for DME providers, causing cash flow disruptions, operational inefficiencies, and missed opportunities to expand your payer network. But these delays don’t happen by accident—they stem from common, recurring issues that can be addressed with proactive strategies.
In this blog, we’ll uncover the root causes of credentialing delays and share practical solutions to keep your credentialing process on track and your business running smoothly.
The Top Causes of Credentialing Delays
- Missing or Incomplete Documentation
- What Happens:
Credentialing applications are delayed when critical documents, such as licensure or insurance, are missing or outdated. - Impact:
Applications may be rejected, requiring resubmission and restarting the approval timeline.
- What Happens:
- Inefficient Tracking Systems
- What Happens:
Manually tracking credentialing deadlines leads to overlooked renewals and last-minute scrambles. - Impact:
Missed deadlines result in temporary delisting or interruptions in provider billing.
- What Happens:
- Payer-Specific Complexities
- What Happens:
Each payer has unique requirements, and failing to meet these standards causes application delays or denials. - Impact:
Providers must resubmit applications, wasting time and resources.
- What Happens:
- Staff Turnover
- What Happens:
When experienced credentialing staff leave, gaps in knowledge or workflow disruptions delay processes. - Impact:
Replacing staff and retraining teams slows down credentialing progress.
- What Happens:
- Lack of Proactive Follow-Ups
- What Happens:
Applications sit in limbo due to a lack of follow-up with payers to track progress or address issues. - Impact:
Delays extend approval timelines unnecessarily.
- What Happens:
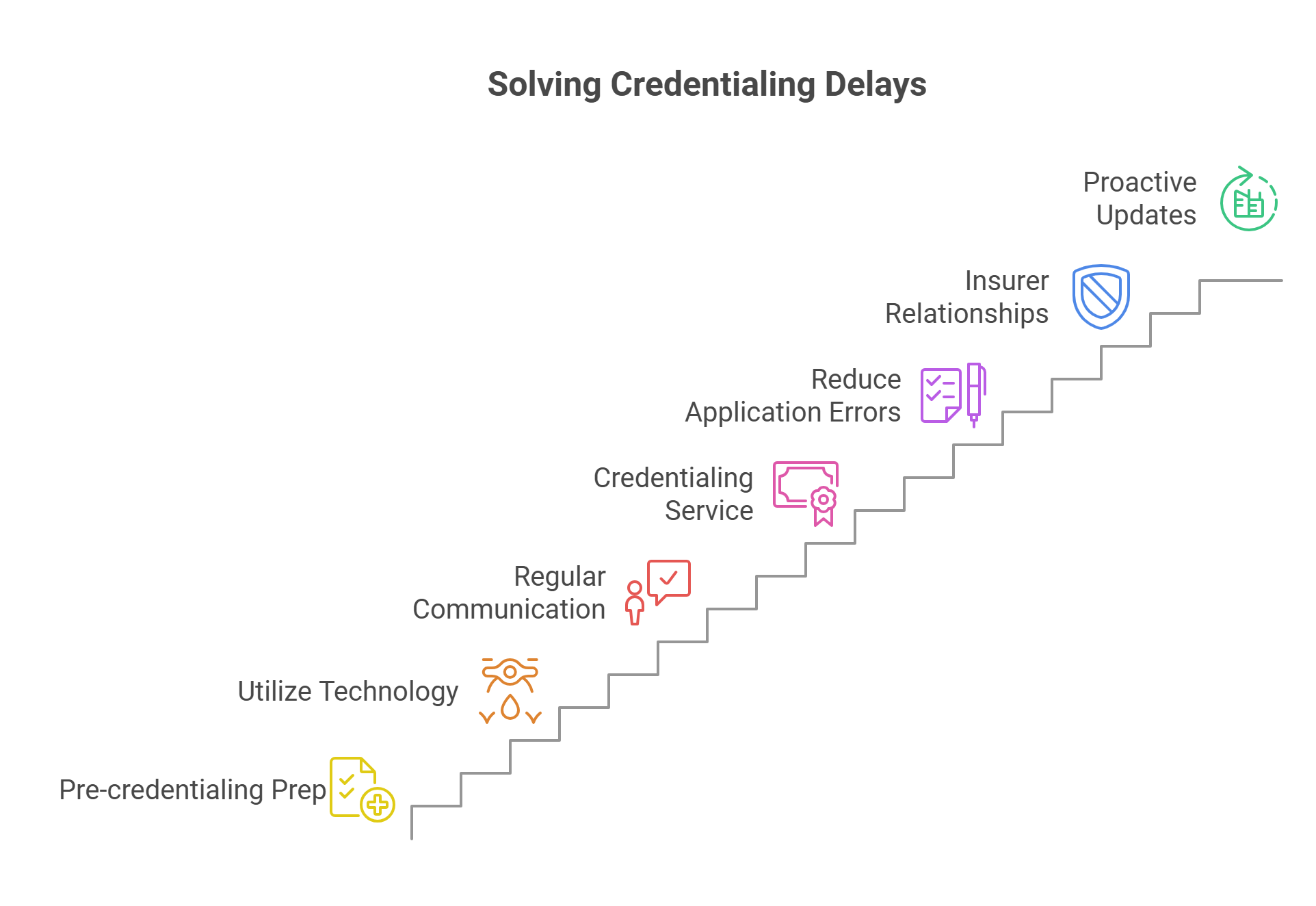
Proactive Solutions to Prevent Credentialing Delays
- Centralize Documentation Management
- Why It Works:
Having all provider files in a single, secure location ensures quick access to complete, accurate information. - How to Do It:
Use credentialing management software to store licenses, certifications, and payer-specific forms.
- Why It Works:
- Automate Deadline Tracking
- Why It Works:
Automation eliminates human error and ensures no deadlines are missed. - How to Do It:
Implement tools that send automated reminders for renewals, updates, and application milestones.
- Why It Works:
- Create Payer-Specific Workflows
- Why It Works:
Customizing workflows for each payer ensures compliance with their unique requirements. - How to Do It:
Maintain a checklist for each payer and assign dedicated staff to oversee critical accounts.
- Why It Works:
- Conduct Regular Internal Audits
- Why It Works:
Proactive audits help identify missing documents or processes that need improvement. - How to Do It:
Schedule quarterly reviews of credentialing files and workflows to catch potential issues early.
- Why It Works:
- Train and Retain Skilled Staff
- Why It Works:
Well-trained staff reduce errors and keep workflows running efficiently. - How to Do It:
Invest in regular training and create clear, documented workflows to onboard new staff quickly.
- Why It Works:
- Establish Strong Communication with Payers
- Why It Works:
Regular communication helps resolve issues and keeps applications moving forward. - How to Do It:
Assign team members to handle follow-ups and build relationships with payer representatives.
- Why It Works:
How WWS Can Help
At WWS, we specialize in eliminating credentialing delays by implementing proactive solutions tailored to your needs:
- Centralized Systems: We help you organize and secure provider data for faster application completion.
- Automation Tools: Our systems track deadlines, send reminders, and minimize human error.
- Payer Expertise: We customize workflows to meet payer-specific requirements and expedite approvals.
Schedule a consultation with WWS today to keep your credentialing process running smoothly:
Schedule a Meeting with WWS.
Conclusion
Credentialing delays don’t have to be a constant headache for DME providers. By addressing the root causes and implementing proactive strategies, you can streamline workflows, maintain compliance, and ensure faster approvals.
Partner with WWS to eliminate credentialing delays—schedule your consultation today!